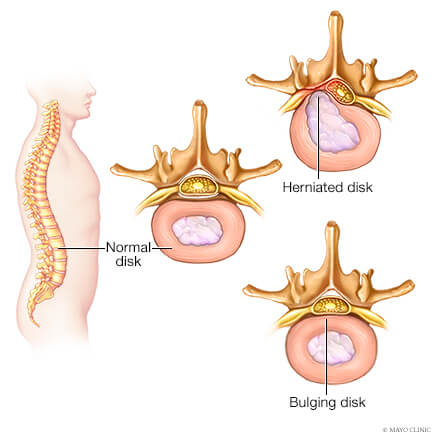
Radiculopathy refers to symptoms that develop when there is compression of a spinal nerve root. Most commonly, the nerve compression is related to a disc herniation or spondylosis (degenerative changes in the spine) and may occur with or without trauma. It is important to note that not all disc herniations cause nerve compression or pain. While any nerve root can be affected, the lower cervical (neck) and lower lumbar (low back) levels are the most common. Because the fibers of one spinal nerve root provide sensation and strength in a specific region of the body, arm, or leg, a compressed nerve will cause symptoms in the region where the nerve provides strength and sensation. Nerves in your neck provide sensation and strength in your arms, while nerves in your low back provide sensation and strength in your legs.


